The Thinking Practitioner Podcast
w/ Til Luchau & Whitney Lowe
Episode 68: Working With Sciatic Pain (with Whitney Lowe and Til Luchau)
Transcript | Subscribe | Comments | ⭑⭑⭑⭑⭑
Or, listen and subscribe on Apple Podcasts, Spotify, Stitcher or Google Podcasts.
Til and Whitney compare notes about their tests and techniques for recognizing, understanding, and working with sciatica, sciatic pain, and similar conditions. Download the free technique handout at https://bit.ly/sciatica-handout-68
Scroll down for the full transcript!
-
- Whitney Lowe's online Clinical & Orthopedic Massage Courses
- Til Luchau’s courses at advanced-trainings.com
Sponsor Offers:
- Til Luchau's 'Sciatica & Disc Issues' training: save 15% by entering "thinking" at https://a-t.tv/onl2208/.
- Books of Discovery: save 15% by entering "thinking" at checkout on booksofdiscovery.com.
- ABMP: save $24 on new membership at abmp.com/thinking.
- Handspring Publishing: save 20% by entering “TTP” at checkout at handspringpublishing.com.
About Whitney Lowe | About Til Luchau | Email Us: info@thethinkingpractitioner.com
(The Thinking Practitioner Podcast is intended for professional practitioners of manual and movement therapies: bodywork, massage therapy, structural integration, chiropractic, myofascial and myotherapy, orthopedic, sports massage, physical therapy, osteopathy, yoga, strength and conditioning, and similar professions. It is not medical or treatment advice.)
Full Transcript (click me!)
The Thinking Practitioner Podcast:
Episode 68: Working With Sciatic Pain (with Whitney Lowe and Til Luchau)
Whitney Lowe:
Welcome to the Thinking Practitioner Podcast.
Til Luchau:
A podcast where we dig into the fascinating issues, conditions and quandaries in the massage and manual therapy world today.
Whitney Lowe:
I'm Whitney Lowe.
Til Luchau:
And I'm Til Luchau.
Whitney Lowe:
Welcome to the Thinking Practitioner.
Til Luchau:
Welcome to the Thinking Practitioner. Books of Discovery has been a part of massage therapy education for 20 years. Thousands of schools around the world teach with their textbooks, eTextbooks and digital resources. In these trying times, this beloved publisher is dedicated to helping educators with online-friendly digital resources that make instruction easier and more effective in the classroom or virtually.
Whitney Lowe:
Books of Discovery likes to say learning adventures start here, they see that same spirit here on the Thinking Practitioner podcast and they're proud to support our work, knowing we share the mission to bring the massage and bodywork community in livening content that advances our profession. So do be sure to check out their collection of eTextbooks and digital learning resources for pathology, kinesiology, anatomy, and physiology at booksofdiscovery.com, where Thinking Practitioner listeners can save 15% by entering "thinking" at checkout. All right. Thank again. Books of Discovery and good day, Mr. Luchau. Good to see you again. We've been sort of off track for a while here doing some solo things. I did some, and you did some.
Til Luchau:
It's been a while since we've been together on the mic, Whitney. Good to see you.
Whitney Lowe:
I missed you.
Til Luchau:
Aw, nice. Likewise, I've been looking forward to this conversation today, a lot.
All right. Good. What is the conversation today?
Til Luchau:
I wanted your ideas and just to mull over my ideas about sciatica, sciatic pain.
Whitney Lowe:
Ah-ha.
Til Luchau:
Yeah. It's one of our most popular courses in my series and I'm teaching a live stream one day, which I'll go ahead and put a plug in for. That's August 12th, 2022, or you can get it later by recording. And, like our other sponsors, you can save 15% if you enter "thinking" at checkout, if you want to go look at that on our site, advancedtrainings.com. We'll put that in the show notes, but enough of that advertisement, I-
Whitney Lowe:
Oh, no, wait. Not quite enough. Tell me more about this course. What are you doing on the live stream? This is you doing this as a broadcast for people all over, right?
Til Luchau:
Yeah. Basically, I'm going to be in Portland, Oregon, teaching a one-day hands-on workshop, complete with lectures and everything. And then we just have a couple of Zoom feeds where people can see different angles of the demonstrations I'm giving and there will be actually people that are practicing on Zoom and we'll be giving them feedback. So we're teaching both Zoom and in-person simultaneously.
Whitney Lowe:
Awesome.
Til Luchau:
Yeah. We did that last year for a class and it was really fun. We had people from all over the world. It's not the same as being there in person, but it was surprisingly effective and satisfying, too.
Whitney Lowe:
Second best. Yeah.
Til Luchau:
That's right.
Whitney Lowe:
To be there with everybody, so yeah. All right. That sounds cool.
Til Luchau:
Yeah. And then I should also mention that we do have a handout for our conversation today. I got a couple things I'm going to put in there. You said you have some stuff.
Whitney Lowe:
Yeah.
Til Luchau:
We'll pull it together after we record and get it up there on our website so you can go download that free PDF if you want.
Whitney Lowe:
Sounds great. Sounds like a plan.
Til Luchau:
So anyway, what is sciatica, Whitney?
Whitney Lowe:
Well, this is a good question because certainly if you look at any of the stuff that's been written about it, this is one of the places where there starts to be confusion. Just to put other plug while we're talking about terminology issues here, are you aware... Well, actually you and I talked about this. Did you see any of the stuff that came out of the recent International Consortium of Manual Therapists Event? They had a virtual event. It was going to be launch. It went to-
Til Luchau:
Yep. I remember the event. What came out of it? What do you think?
Whitney Lowe:
Well, one of the big things that came out of that was a discussion about terminology, about the need for consistent terminology across manual therapy professions. And that's just something that it's great to see some work being done on this, and some things to move stuff in certain directions. Because this is a perfect example of when you have a term that is not agreed upon and is not accurately defined, it's open to all kinds of different interpretations about different people. And the term sciatica gets bandied about quite a bit, especially as a lay person's term for describing any kind of pain down the lower extremity, and that really isn't accurate. I mean, ideally, we would like to let the term be defined by pain in the sciatic nerve distribution that is specifically deriving from sciatic nerve involvement. And so that's one of the more-
Til Luchau:
Oh, boy. Okay, good. We're going to have stuff to talk about. This is good.
Whitney Lowe:
Yeah.
Til Luchau:
Okay. So how would you define it? Is that how you define it, pain in the sciatic nerve distribution?
Whitney Lowe:
I would say pain in the sciatic nerve distribution that is derived specifically from sciatic nerve involvement, because you can have pain in the sciatic nerve distribution that's not from the sciatic nerve.
Til Luchau:
All right. So that opens up the debate about the derivation of pain. What is the cause?
Whitney Lowe:
Well yeah.
Til Luchau:
But you're saying, okay, so where is the sciatic nerve distribution area?
Whitney Lowe:
Yeah. So this is going to be a wide area, all the way from the lumbar, depending on which branches we're talking about, but this could anything from the lumbar region through the gluteal area, and of course down the back side of the leg and all the way into the foot, depending on which different nerve branch that we're talking about and where it branches off of there. But in general, we're talking pain down the backside of the thigh, gluteal region, and down the backside of the thigh, into the foot.
Til Luchau:
Gluteal region, otherwise known as the butt.
Whitney Lowe:
Yeah. Yeah.
Til Luchau:
And maybe some low back. Is that in there at all?
Whitney Lowe:
Yeah, certainly. Oh, certainly. Yeah, yeah.
Til Luchau:
All right. So pain in the butt and back and leg. We're getting technical. We're already getting to the weeds, which is really cool, but I just want to say this topic, for nomenclature reasons, but also for other philosophical reasons, is really an interesting poster child of a condition because there are some amazing things we can do to help, and yet there's times that it's not how we think we might help, too. [inaudible 00:06:20]
Whitney Lowe:
And you're going to explore that with us a little bit, right?
Til Luchau:
Yeah. I'm going to explore that with you. I'm going to ask you about it, too. But people come and it hurts and they just want it to stop and often we can, and even when we can't, there's amazing things we can do. Anyway, you're saying it's pain in this region.
Whitney Lowe:
Yeah.
Til Luchau:
You're tying it to the sciatic nerve itself.
Whitney Lowe:
Yeah. And again, there are people who say, "I've got sciatica," and basically they have pain either in their butt or down their leg. So I'm not going to say, "Well, no, you don't have sciatica," if it's pointing to, there may be some other sort of derivation or source of that pain. I certainly clinically wouldn't negate that experience and just say, "Well, let's see what we can do with this."
Til Luchau:
There you go. You don't want to argue with them about what they're calling it. Another way I've heard it talked about is it's sciatica, or sciatic pain is a symptom, it's not a condition, per se. That it's something that shows up as a result of something else going on.
Whitney Lowe:
Yeah, I think so.
Til Luchau:
And it has become a colloquial term just to mean what you said, pain in the back, the butt.
Whitney Lowe:
I think I may have talked about this in one of our earlier episodes. I'm curious if this has ever happened to you. I had a situation where I was in clinic work. This was back when I was in Atlanta and working at Emory. And because Emory was a really prominent medical center in Georgia in the South, people would come from all, especially rural areas where they didn't have access to really good high-quality orthopedic care. They would come up to Emory. I had this guy come in one day and he was complaining about the leader down his leg. I said, "I'm sorry, what did you say?"
Til Luchau:
The leader down his leg, right.
Whitney Lowe:
The leader. I had never heard that term before so I had to have him describe that to me. And apparently this is a colloquial term in certain rural cultures about pain down an extremity. I don't know where the term comes from. Have you ever heard that term before?
Til Luchau:
I've heard it in fly fishing. You got a leader. But no, I don't know about that pain down a leg at all.
Whitney Lowe:
What does it mean in fly fishing?
Til Luchau:
It's like the thing the hook's tied to, you know that last little bit of line there.
Whitney Lowe:
Yeah.
Til Luchau:
If I know my terms.
Whitney Lowe:
I wonder if that is any relationship to how this came about or was derived. Anyway, I had to ask for clarification about that. Like, I'm going to have to get a little clearer on what this is. I've never heard this before, but-
Til Luchau:
Well, maybe there's something educational we can extract from that. It is important to ask people what they're actually experiencing and not just take their terms at face value and think that we know what they mean.
Whitney Lowe:
Yeah. Certainly. Because, again-
Til Luchau:
Dial down their experience.
Whitney Lowe:
Yeah. And people be using those terms different ways for different things. So always good for clarification purposes.
Til Luchau:
What else do you want to say about definition?
Whitney Lowe:
Well, so again, just as a reminder, a brief anatomy reminder, that the sciatic nerve is a big sucker. Especially if you look at some of those dissections of the sciatic nerve, it's about the size of your pinky finger. So I mean, that is one big hunk of nerve. It comes off of the nerve roots from L4 off the lumbar plexus, all the way down to S3 off of the sacral plexus, and combined fibers all joining together to make up that nerve. And do remember it has kind of two primary divisions that sort of split, usually around the knee, so those fibers can be sort of blended together and then eventually separating farther down in the lower extremity as well.
Til Luchau:
So it's a fat nerve. I'm going to highlight what you said, look at your pinky finger. You got a nerve in your backside that's that big around and it has some of the longest neurons in the body, too.
Whitney Lowe:
Absolutely, yeah. Yeah. And, interestingly, as you noted here, when you talk about having some of the longest neurons, a lot of people aren't aware that those individual nerve cells that go all the way down the whole length of those nerves in our extremities are single cells, all the way from nerve-root level to the termination of those nerves. So when you talk about the digital plantar nerves in the toes, those nerve cells go all the way up to the lumbar nerve roots. And to me, I think that's just incredibly fascinating.
Til Luchau:
It is like a three-foot long nerve in a human. 15-foot long nerve in a giraffe. They have a 15-foot long sciatic nerve. So that means, I'm sorry, I don't mean to steal your thunder at all, I hope I'm not butting in, that means they're vulnerable. Because they're so long and so big, they're vulnerable to certain processes that smaller, more protected nerves might not be.
Whitney Lowe:
Yeah. And elaborating on that point, when you mentioned the length of those nerves, we're not talking just about the length of the nerve as a whole, we're talking about the individual cells, the individual nerve cells in there.
Til Luchau:
The axion.
Whitney Lowe:
The reason that that is so important is nerve cells derive a lot of their function and are responsible for transmitting their own nutrient proteins inside the nerve cell through the flow of something called axoplasm. Now, if that axoplasmic flow is impaired by, let's say, an obstruction or some kind of thing that's interrupting the smooth pathway of that nerve somewhere along its path-
Til Luchau:
Something steps on the hose.
Whitney Lowe:
Something steps on the hose. Exactly.
Til Luchau:
Like a little tube. The nerve is like a little tube with its own axoplasm nourishing the nerve.
Whitney Lowe:
Yeah. So once you step on that hose, then everything distal to that point is somewhat nutritionally deficient and therefore potentially sensitized and more vulnerable to other symptoms arising. That's where that whole process comes from that's referred to as the double or multiple crush phenomenon. Especially when you get these very long nerves, they are highly susceptible to that kind of thing.
Til Luchau:
Okay. So can I put in a plug for fascia right here?
Whitney Lowe:
Absolutely.
Til Luchau:
Those hoses, those tubes, are basically fascially wrapped nerves, or there's a layering system within the nerve that is the endoneurium, epineurium perineurium, that basically forms that hose-like structure. And so it's subject to all the things other fascia is, which can be healthy perfusion, caring of vasculature and lymph vessels, including probably lymph flows directly within the tissue. And it can get either scarred or adhered or thick or dense or less perfusible, and probably we're thinking that can cause nerve symptoms, too, just the quality qualitative change in the fascial component of the nerve itself.
Whitney Lowe:
Yeah. And we'll expand on this a bit later, but I do want to reiterate that, especially some of these things that you're talking about, do not show up well on high-tech diagnostic studies like MRI.
Til Luchau:
Oh, yeah.
Whitney Lowe:
So it's very, very difficult to identify those through traditional means. And to me, that's one of the great values of some of the things that we do as soft-tissue therapists is investigating some of these things through much more thorough and comprehensive manual evaluations and looking at these things in functional capacity a lot more than just what shows up on the MRI.
Til Luchau:
Well, we'll talk about, at some point, and if I don't talk about here, we'll put it in a handout, about different sorts of interventions that can leverage that tube-like architecture, that can help that hose flow better. Now, you have something in there about true sciatica and the sciatic nerve. What do you mean by that?
Whitney Lowe:
This is basically, essentially, what we were talking about earlier, which is true sciatica being something where there is impairment or irritation of the sciatic nerve or it's branches, being differentiated from the "sciatica," in air quotes, that is just simply pain down the backside of the leg.
Til Luchau:
Oh, I see.
Whitney Lowe:
It might be coming from other causes.
Til Luchau:
Because I've heard a distinction made between true sciatica and pseudo sciatica.
Whitney Lowe:
Yeah. And I would call the pseudo sciatica, those things that are not sciatic nerve derived, but-
Til Luchau:
I've heard pseudo sciatica referred to piriformis syndrome. True sciatica being nerve root, and any other insult or irritation to the sciatic nerve elsewhere along this pathway being pseudo sciatica.
Whitney Lowe:
Yeah. I've heard that same kind of distinction. I'll have to say, personally, I don't like that distinction.
Til Luchau:
Why?
Whitney Lowe:
Because the piriformis involvement, if we're talking about the sciatic nerve, which is the most common way in which the sciatic nerve is impaired in that region by muscle tissue, that's impairing the sciatic nerve, as is the nerve root or an obstruction in the lumbar region. And it seems more relevant to me to make a distinction between those things that are actually impairing the sciatic nerve from those that aren't. And that to me would be pseudo sciatic.
Til Luchau:
That's the distinction you make. Okay.
Whitney Lowe:
Because it's really hard to make a distinction between, okay let's talk about the sciatic nerve is irritated up here in the lumbar nerve root versus being irritated in the piriformis region. I mean-
Til Luchau:
Absolutely.
Whitney Lowe:
... it's certainly helpful to do that, but it's still the sciatic nerve.
Til Luchau:
Well, I mean, chiropractor call it type one or type two. I've heard it called true or pseudo, but again, the distinction there in those systems that I've heard are different than what you're saying, Whitney, is that it is either nerve root or not. Either nerve root or peripherally, more distal down the nerve. And again, that's useful for us therapeutically because we can start to think about where, if there is one location, where there might be an issue. But on the other hand, there's limitations to that division as well. In my class I do a distinction between axial and appendicular, but it's often the case that we troubleshoot both. It's hard to tell exactly where it is, but we can do it empirically. We can do at different kinds of movements and things like that to help narrow down, to see what helps, at least, even if we don't know the exact location.
Whitney Lowe:
So tell me about that distinction between axial and appendicular. Is that just kind of like what we were talking about here, too, in terms of being in the torso, spinal region versus non or something.
Til Luchau:
Axial being nerve-root related, is it the nerve roots of the feeder nerves that become the sciatic nerve? Is it right there where they exit the spinal canal that they're being either compressed or irritated? Or is it somewhere downstream? That's appendicular. And the only reason I think I keep that distinction is because it does kind of parallel what I understand about the conventional division, but it also helps us, again, start to target where we think we might start and see what happens.
Whitney Lowe:
Right. I think that's a good distinction. I like that, axial versus appendicular, and that does sort of get us thinking, too, about where we're going to potentially target with other treatment strategies and things like that.
Til Luchau:
Great. Should we talk about how we would start to narrow that down, how we might recognize what's going on?
Whitney Lowe:
Yeah. We put some notes up here and, as we're talking about this, I think what I'd like to do is talk first about some of these other things that might be confused with sciatic nerve involvement, and then we talk about how do we specifically recognize it because it'll help about when we talk about some of those distinctions.
Til Luchau:
So differential diagnosis kind of thoughts. Great.
Whitney Lowe:
Yeah. I've got a list of a few things that we know, and this would be sort of in that category of pseudo sciatica, of things that can mimic sciatic type pain and prove very similar type of symptoms. So they run the gamut from myofascial trigger points, especially in the gluteal muscles. We see a lot of those pain referral patterns from, especially the hip abductors, gluteus medias and minimus doing that. And some of the other gluteal muscles also putting that pain down the backside of the leg.
Whitney Lowe:
And then you mentioned earlier, too, piriformis involvement, and this is one that people don't tend to make a strong distinction about, but I've also heard pretty common misconceptions about this when you talk about that whole pseudo sciatica thing, and that's involving the potential compression of another branch of nerve off this area called the posterior femoral cutaneous nerve.
Whitney Lowe:
And I don't know, tell me maybe if you have heard this before, I've certainly heard this numerous times, people saying, if you've got pain going all the way down your leg into your foot, then that's a nerve root problem in the sciatic nerve. If you've got pain just down to your knee, then that's a piriformis entrapment of the sciatic nerve.
Til Luchau:
Yeah. That's what chiropractors are taught, and there is some good evidence. I think the trend is toward that. If it's below the knee, it's probably a nerve root. Valtuk said the opposite, and he was a pretty influential spinal researcher who did a bunch of some of the work we're still using to understand spinal pain. By the way, spinal pain, we're going to talk to Dr. Stewart McGill in an upcoming episode. So I just got to say anything I say about the back is going to be tentative. He's like Mr. Back pain.
Whitney Lowe:
Super excited about that conversation. We'll see how well that wraps into what we're talking about here as well.
Til Luchau:
Yeah. So basically, the takeaway is there's disagreement in different disciplines. Chiropractors will say below the knee, yeah it's nerve root. Others say, no, it's if it's below the knee, it's probably not. Who knows?
Whitney Lowe:
And one of the reasons I wanted to bring that up is that I don't agree with that classification and I think that comes out of a misunderstanding, I think, of some anatomical factors that may play into this. For example, the posterior femoral cutaneous nerve is, as it's name indicates, a cutaneous nerve giving sensation to the posterior thigh and it terminates around the knee. It doesn't go below the knee. If you compress the sciatic nerve with the piriformis muscle in the gluteal region, you can definitely produce lower extremity symptoms down below the knee.
Whitney Lowe:
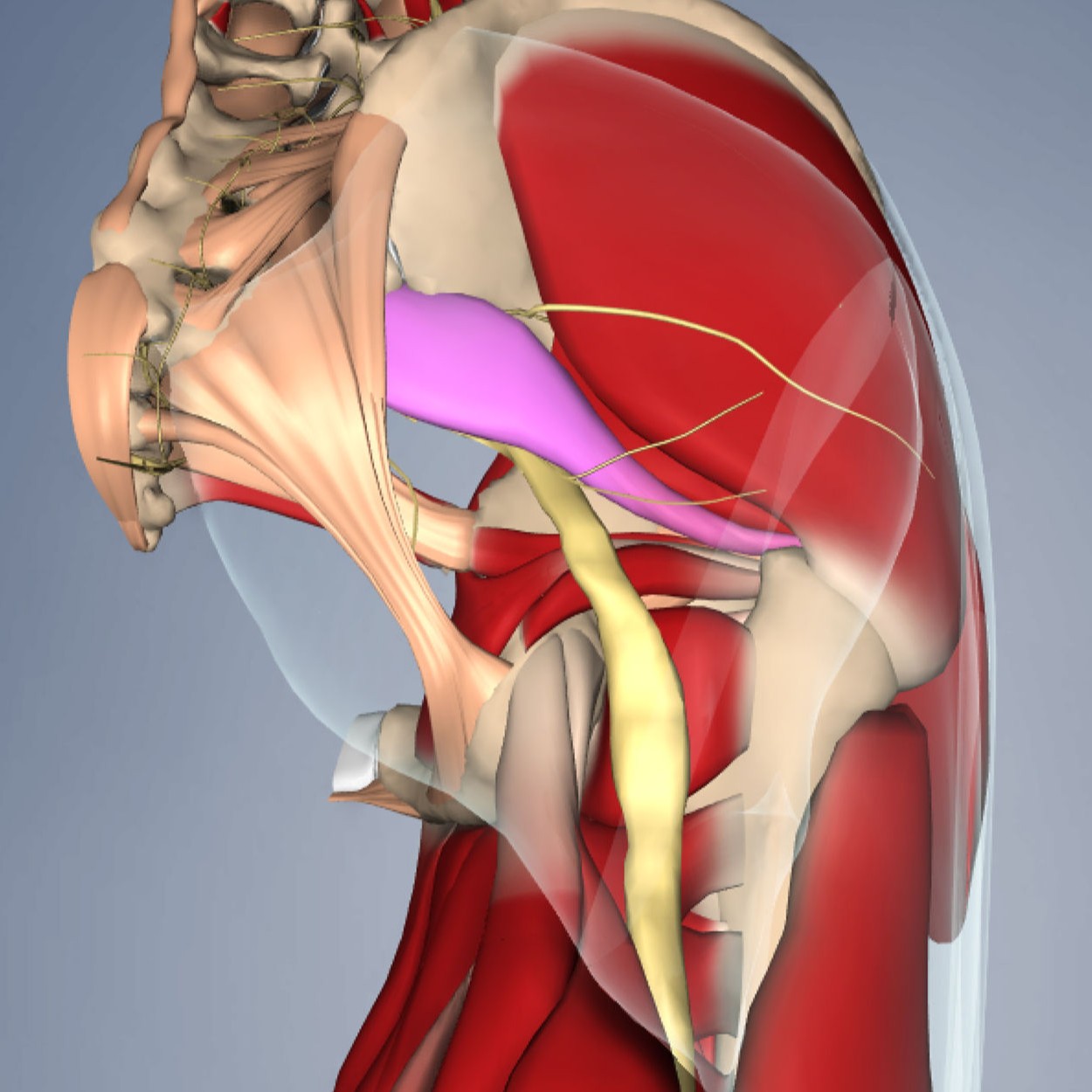
And I think in many of these instances where the piriformis muscle is involved, we are actually entrapping the posterior femoral cutaneous nerve and not the sciatic nerve, and that's why those symptoms only go down to the knee, because of that particular nerve. And if you look at an anatomy reference, and maybe we'll put a picture of this in a handout-
Til Luchau:
Yes, we need a picture.
Whitney Lowe:
... we can see how close that posterior femoral cutaneous nerve is to the sciatic nerve. It's just right next to it. These structures tend to get compressed against the sacrospinous ligament in the pelvic region, and they're both very susceptible to that. That's one of the reasons that I'm not quite sold on that whole thing of it's piriformis if it only goes down to the knee. Well, it might be piriformis, but it might not even be the sciatic nerve. You could be looking at PFCN entrapment there as well.
Til Luchau:
PFCN?
Whitney Lowe:
Yeah. Posterior femoral cutaneous nerve.
Til Luchau:
Nice. Well, I got to just ask, how does it matter?
Whitney Lowe:
Yeah. So from a treatment perspective, I think that either one of these is going to drive the same treatments, as far as I'm concerned, which is primarily, we're going to try to target the gluteal and piriformis region. What it tends to do, I think, is sometimes not scare people as much because when they hear about sciatic problems, that carries a lot of baggage for people sometimes.
Til Luchau:
Well, it's pretty commonly associated with disc problem. For a lot of people, it's a sign of disc issues and the classic PTs are taught if you can reproduce sciatic pain, then it means, under certain circumstances, there's a disc issue. That thinking is loosening, that correlation in people's mind is loosening culturally. But still, sciatic pain does sound kind of bad and has lots of associations to people.
Whitney Lowe:
Yeah, certainly. And then just a couple other things, sometimes, and again, this is not a real strong correlation, but there have been some indications that irritation of the zygapophysial, or facet joints of the spine, can produce radiating pain symptoms in the gluteal and/or lower extremity region, as well. As can sacroiliac joint dysfunction also produce some of those kinds of symptoms. And the reason I wanted to talk about a couple of these things before we talked about identifying, making some distinctions about how to identify is because this is one of the ways in which there's more specific evaluation procedures are helpful to distinguish between true neural involvement and some of these other things that might be joint related or something like that.
Til Luchau:
Okay. I almost named my dog zygapophysial.
Whitney Lowe:
And then you can call him Zyg instead of Zig, or something.
Til Luchau:
Yeah. Something like that. But basically, facet joints, you're saying, can mimic or be similar to the sciatic kind of symptoms, as well as sacroiliac joint dysfunction or sensitivity. While we're doing the list, from my side, I should stick in, you mentioned sacrospinous region, but also sacrotuberous related issues, you could say. Or at least those are the places we can work, that seem to make a difference. They're on my map of things to check, for sure.
Whitney Lowe:
Yeah.
Til Luchau:
Anything you want to say about that Whit?
Whitney Lowe:
No, I think those are the ones that I want to bring up as potential confusing identifications that may be mistaken for sciatic nerve involvement. And we did mention, I think, or maybe we didn't mention, in terms of nerve root involvement, there are a couple of things when this is a sciatic involvement at the nerve root level, that this may occur from intervertebral disc herniations, other types of obstructions, spinal tumors, bone spurs, stenosis. Those are factors. Sometimes spondylolysis or spondylolysis, they generally break down in the articular structure of the vertebra itself. Those are all factors that may also cause nerve root involvement.
Til Luchau:
So those are all things that can put mechanical pressure on the nerve root, where the nerves are exiting the spinal canal.
Whitney Lowe:
Yeah. Yeah.
Til Luchau:
Okay. I should add, before I just ask a different question, there's also some speculation about muscles in that region that run parallel to the nerves, unnamed muscles that have been observed in dissection that seem to be responsible, maybe, so speculatively, for retracting or stabilizing those nerves as they slide in and out of those canals. So if they're muscles, the theory goes, maybe they get bigger or get inflamed or something like that. But certainly there's fascial sleeves. There's the dural tube that goes around the nerve and then the perineurium around the nerve, there's different fascial sleeves there that can also be part of, even if it's not a bony overgrowth or a positional problem, that's closing the foramen. There can be soft issue contents in that foramen that can get bigger, you could say. Maybe there's muscles in there, maybe not, or fascia, maybe the fascia can get denser or inflamed or thicker and cause a mechanical compression, stepping on the hose right there, for example.
Til Luchau:
And then there's a debate about whether you even need compression to have the sciatic nerve symptoms. Peter Sullivan, et cetera, saying that actually it's a question of irritation. And often, conventionally, we assume that compression equals irritation, but that you can have irritation of the nerve without having compression of the nerve. And that this holds true in surgical interventions where often, well, probably manual therapy, too, often we'll do something that seems to relieve the direct compression on the nerve but there's still pain there sometimes, unfortunately.
Whitney Lowe:
So those other things that might cause irritation of the nerve other than compression.
Til Luchau:
Yes.
Whitney Lowe:
Examples being like chemical mediators-
Til Luchau:
Inflammation.
Whitney Lowe:
... inflammation.
Til Luchau:
My favorite.
Whitney Lowe:
Your favorite thing.
Til Luchau:
My favorite thing. So it could be local inflammation of some of those connective tissue structures that make up the nerve. It could be, and there's some good evidence for this, neighboring structures like your facet joints, like spinal ligaments and things like that could be inflamed themselves, and that inflammatory process also irritates its neighbors just through the direct chemical interaction or immunological interactions with the neighboring structures. It's a shift in thinking for me, too, when I started realizing that sciatic pain was a result of sensitization and maybe not always mechanical compression. That changed my therapeutic approach, too.
Til Luchau:
Because I found this from the beginning. A lot of times I would do things that would clearly help there be movement or more spaciousness or different things there. And the pain would still be there sometimes. Sometimes it would go away magically. Other times it's like we did everything and it still hurts just as much. Yeah. So that just made me start to think about pain as an independent variable, like pain is something different than what's going on, either tissue-wise or structural-wise. And there's some interesting... Can I tell you a little piece of trivia?
Whitney Lowe:
Of course. I love those.
Til Luchau:
This is, I'm looking at my notes here, which turned the page. Let me get there. Okay. Yeah. This is Tom Justin's story. He says 1958 Smith and Wright, they published a paper on this. They were spinal surgeons. They wanted to tease apart this sensitivity compression thing. They did disc surgeries and they would sew in pieces of thread looped around the nerves on both sides. Have you heard about this one?
Whitney Lowe:
I have not.
Til Luchau:
So the thread was coming out of the skin, they'd leave it extending out of the incision on both sides. And then afterwards they would monitor the sensitivity of the nerve and the healing process. So they took away all of the compression of the nerve through the surgical process. They'd leave a little thread attached, looped around the nerve itself, and then every now and then they would very gently tug on these threads to see if the nerve was still sensitive and they'd use the unaffected side as a control. So the unaffected side wouldn't produce any pain, but in many patients for days afterwards, the smallest tug on the nerve would still produce the same pain, even though all the compression was gone.
Whitney Lowe:
Yeah.
Til Luchau:
So their takeaway was the nerve is still sensitized and that's what's responsible for the pain phenomenon but not so much the... So the hose get stepped on, but whatever changes in the nerve or changes in the brain around the sensation of the nerve are responsible for the pain. And that can be independent of the nerve compression itself.
Whitney Lowe:
Yeah. And I think this is something we will probably explore in a little bit greater detail when we have that conversation with Stuart McGill here, coming up too, because this is certainly his realm. I've heard him talk a number of times about this in terms of the necessity of teaching people about more optimal movement patterns that really can alleviate a lot of pain. Like when you have a certain type of thing with your back that causes sciatic pain shooting down your leg, or whatever, every time you lean over the sink to brush your teeth. And then that just perpetuates into, I know when I try to lean over to do something else, this is going to hurt. And that whole sensitization thing gets really out of whack. There's a lot of things that I think we can play a part in, in terms of turning that around, but people have to remember this generally doesn't happen quickly. There's oftentimes going to be a little bit more time involved with making it occur or making it happen.
Til Luchau:
Well. Yeah. I can't wait to hear what he says about his sniff and his different kinds of things he does to help people stabilize in his model, around the nerve, but then for me, teasing it apart from... My goal is to help people with their pain, of course. That's what they want, too, but it doesn't always happen right away. Even if I've done the tissue part, that there's still a neurological part, often. The nerve is still, or the brain is still sensitized. And that oftentimes that takes a little more time, just time for the body to adjust.
Til Luchau:
And then on the other hand there's times when that doesn't seem to go away, honestly. As confident as I am in my treatments and as much as I would like to say, this is an effective approach, which it is, there's times it just doesn't seem to go away. And sometimes helping people think about it in terms of sensitivity or irritation more than a compression, can be a more helpful reframe, can be a way to realize your nerve is sensitized, it's irritated, so it hurts. It may or may not be because it's compressed. We don't really know.
Whitney Lowe:
Right. I also wanted to draw back a second on something you said a few moments ago and highlight this because it's something that I think a lot of people may not be aware of or may not think about a lot. If you look at the traditional orthopedic literature around sciatic nerve pain, it is strongly, strongly biased towards looking at functional mechanical stresses on nerve roots, discs and some of those other major structural things. You've mentioned a few moments ago and we have sort of learned more in recent years and I think it is just still grossly underrepresented, the role of a lot of these soft tissues in some of these pain complaints. And especially as we look at the degree of neural supply from myofascial tissues in particular into the central nervous system. I still think they have been very underrepresented and under-recognized as contributors to various types of nociceptive overload that people experience. And of course, that's of particular interest to us, as manual therapists, who work with a lot of soft tissue stuff.
Til Luchau:
Totally. It is for me. I mean, whether you're thinking fascially, or you're thinking neuro-centrally and, pain science or fascia science, whichever or both, there's a whole lot of different ways to help or go after sciatic pain. A lot of different things that aren't necessarily provided in other ways.
Whitney Lowe:
Yep. Yeah.
Til Luchau:
That said, if someone comes to me with severe intractable sciatic pain, or if there's certain tests we do like a Lasegue test or something that shows pain in certain ways. I want them to be under the care of another primary care physician, for sure, but maybe a specialist, either a neurologist or physical therapist, somebody, because there might be some perspectives that I use that are helpful, but it's not to say that I know things that the other people... that they shouldn't come to be getting conventional care as well, too. That's so important, especially for severe intractable pain.
Whitney Lowe:
Yeah. And that's a very good example. To give another example about that, let's say a person comes in with pretty severe radiating sciatic-type symptoms down both lower extremities and the practitioner says, "Well, my teacher told me we can do some soft tissue work on this and help them out a little bit," and so-
Til Luchau:
It might be true.
Whitney Lowe:
... I'll take them on and not refer them or whatever.
Til Luchau:
Well that part, no.
Whitney Lowe:
And that person needs to be seen by an orthopedist, because they may have a central protrusion and Cauda equina syndrome, that something's pressing on both sides or directly on the spinal cord and that's why you're getting bilateral symptoms. So again, that's another good example of why it is helpful to be able to know some of these things that are big red flags that we do want to send elsewhere.
Til Luchau:
So both-side pain being one of those. I'll put it in the handout about the Lasegue, or straight-leg test, if we don't talk about it here. But if someone does that test, they lift their leg, and the other side hurts, that's like a red flag. That's like a go to jail kind of thing, go to the other practitioner, check this out. Something's going on there that's not good.
Whitney Lowe:
Yeah. That's something that's often called the well-leg test and it's fascinating. It, again, helps to have a little bit more understanding of neural dynamics, but if you do something on the unaffected side and it increases those symptoms, it's because of the overall neural pull affecting that side where there is a potential problem. And this usually indicates something that is highly sensitized and probably needs to be seen by somebody else as well. It doesn't necessarily mean that we can't do some things with people, but they should certainly... I agree with you in that situation, I'm going to refer that person out for additional evaluation as well.
Til Luchau:
Or yeah. That's the well-leg thing, but I'm talking about, say, lifting the affected leg and the pain starts on the unaffected side.
Whitney Lowe:
Oh yeah.
Til Luchau:
That can be a sign of some spondylolisthesis or some movement in there that needs to be under some care, some serious care there.
Whitney Lowe:
Yep. I agree.
Til Luchau:
Okay. What's next?
Whitney Lowe:
Well, you mentioned a couple of things. You mentioned the Lasegue test, also called the straight-leg raise test. That is probably one of the most common physical examination procedures that's often done for this type of thing. We'll put this picture on the handout and describe it a little bit. The client supine on the treatment table and then the leg is raised to see if that increases those sciatic nerve symptoms. Because after about 60 degrees of hip flexion with the knee extended, you're pulling on the sciatic nerve and putting some tension on it and pulling potentially the whole neural structures against any protruding or obstructing tissues or obstacles along the path that might sort of reinforce or reinvigorate those symptoms that the person is experiencing. And then we might compare that against some other things that might, for example, isolate the piriformis muscle and its potential involvement. There's a couple different tests for the piriformis involvement, as well.
Til Luchau:
Let's talk about those, but let's go back to the... You say Lasegue, I say Lasegue, or the straight-leg raise test. Super commonly used in orthopedic examinations. Really well researched. Done with all the different parameters. Pretty high degree of both sensitivity and specificity. And you said pulls on the nerve root. Yeah, it also can pull on the dural tube, for example. And there's some cool work that David Butler republished in the '90s, David Butler of the Noigroup, Pain Science Group, from Brieg 78, just showing... Brieg went sewed little markers onto the sciatic nerve roots and raised the leg and you could see those markers coming in and out, like an inch or more out of the nerve exits.
Whitney Lowe:
Yeah.
Til Luchau:
So you're actually sliding nerves just by lifting the legs, in other words.
Whitney Lowe:
Yeah, exactly. And also back to what you said a moment ago, too, about the whole dural tube involvement, the very last step of that test involving cervical and head flexion-
Til Luchau:
Flexion, yep.
Whitney Lowe:
... pulling the upper end of the whole dural tube and further sensitizing those maneuvers. And again, David Butler certainly has done some marvelous work. And Michael Shacklock is another who's done some-
Til Luchau:
Neurodynamic stuff.
Whitney Lowe:
... excellent illustrations of those neurodynamic tests there, so those are very good resources to learn a little bit more about that stuff.
Til Luchau:
I use those a lot with clients to help me get a sense, not to tell them whether or not they have this or that, but to help me as a practitioner start to put together a working hypothesis about where I'll start. If that straight-leg raise test shows some sciatic pain, reproduces their pain, then I am thinking nerve roots. If they drop their head forward or they flex their spine, I'm also thinking nerve roots, but probably, like you said, pulling from above. If it doesn't reproduce their pain, then I'll go on to the piriformis test that you were starting to talk about.
Whitney Lowe:
Yeah. And another thing that I find value in doing some of these procedures is that, for example, if you do that straight-leg raise test and you find it highly sensitized, we can use this as a means of saying, "Look, if you're going to sit down and tie your shoes, bend your knee, don't do it with your knee out in front of you here and straighten down, because every movement that you do that lights that sciatic nerve up further sensitizes the system." So we can use that as movement coaching for encouraging people to do things that don't irritate those structures further. Because now we're just zoning in and identifying what are the problematic positions and/or movements that really cause them further challenge.
Til Luchau:
Yeah, I like it. I might have a little different spin on it. I'll tell them to play with the edge of it. In this model, we do want to light it up a tiny bit in a controlled way and in a dosed way. So bend over like you're going to tie your shoes and find the edge of that place that sensation starts, and now back off, and now wiggle your toes, and now breathe, and now think of a joke or whatever. Do something that just helps shift the context around that. So playing around the edges of the thresholds where that pain starts. Rather than just like a straight "Don't do that, avoid that," which could be alarming or make people feel more protective or more fragile over time, too.
Whitney Lowe:
Yeah. And that's a really good point I would like to clarify, in saying that, that my encouragement would be to them, is that at different stages, different things are going to be appropriate. When it's in the really bad flared up stage, that's where I'm going to tell them "Don't do that." But as they begin to get a little bit more movement, I'm going to do exactly what you said, just tell them to push the envelope a little bit, but we don't want to do it when it's really in that flared up stage because that will, a lot of times, increase the neural sensitivity.
Til Luchau:
Well, basic inflammation approaches, meaning if it's inflamed, we treat it carefully. And this isn't the place, and, like you said, to stimulate or increase, willy-nilly at least, the inflammation. We want to calm it. We want to increase the adaptive range around it. And some of that's through just rest and avoiding irritants, movements that irritate, and some of that can be re-contextualizing or perfusion or hydration, different things like that
Whitney Lowe:
Yeah. And one of the other I want to talk about for just a second, draw back to our discussion of using these procedures from an evaluation standpoint. I also find these really valuable as a marker of progress for people. So, when you set a baseline at the outset, like they only get their leg up to about 45 degrees or less of hip flexion until that really just lights up and then six weeks down the line we're working, let's take a look at this again and see where we are, and all of a sudden they realize, oh wow, I can get farther than I did before. That's a nice, objective measure of improvement that really stimulates positive thought and positive momentum about making progress in there.
Til Luchau:
Well, it gives another marker besides just, "It hurts," too. Because "It hurts" is hard to track over time. I mean, I do everything I can to avoid that being my only measure of success because, as amazing as we can be about helping people with pain, if that's our only yardstick, it's tough. So things like, "Can I move more? Can I move before it hurts? Can I move in different ways, in spite of the hurt?" All those kinds of things are also great alternatives.
Whitney Lowe:
Yeah. Yeah. I love it.
Til Luchau:
And that test. You're talking about treatment. There's so many ways you can use that test, raising the straight leg or dropping the head, as a way to therapeutically help the nerve, too. I mean, I got a couple in my course from Greg Lehman, he kind of gave me the illustrations about his versions of that. But if you just YouTube sciatic slider or slump slider or sciatic tensioner, you'll see dozens of variations. There's people juggling and doing this exercise. There's people peddling a bicycle and doing this exercise. Lots of ways that to adapt that test into a therapeutic intervention as well.
Whitney Lowe:
Yeah. Yeah. And you're going to explore some more treatment strategies with us here on some of those things, as well, some other-
Til Luchau:
Well, yeah. There's a lot that are based right around that test, that we can use the sensitivity, they find, to shift the thresholds or to hydrate the nerve or to increase mobility, whatever the goal is.
Whitney Lowe:
Yeah. Yeah.
Til Luchau:
And there's more there's manual manipulations, as well. I'll put it in the handout, at least.
Whitney Lowe:
Is there anything, because I know you're very well immersed in and really well versed in these understandings of neural inflammation issues. Is there anything that we can do that will lessen impact or decrease the neural inflammation that may be going on from irritated neural structures in this way?
Til Luchau:
That's such a good question. Is there anything we can do to lessen the impact or decrease the bother or the pain of neural inflammation? There is so much we can do. There's not a magic muscle we massage and it all goes away, often. Sometimes there is. But there's, I'll put it in the handout, there's at least six different ways to work with neural inflammation and we've already named or implied a couple of them. One is simply reframing it from being "You're damaged" to being "You're protective." I mean, these aren't damaged signals. These are protective signals.
Til Luchau:
For example, helping people think about their pain in different ways. It can be that subtle. There are direct mobilizations we can do that help change perfusion, change the function of that hose in a way that probably helps resolve things immunologically or inflammatory, where the inflammatory processes get to cycle through and resolve as well. And then six other things in between, or four other things in between those two, whatever.
Whitney Lowe:
Nice. Yeah. And you'll include that stuff in the in the handout for us.
Til Luchau:
Yep. Yep. I'll put those, the list of six, in there and it'll spur some thinking.
Whitney Lowe:
Yeah.
Til Luchau:
You mentioned piriformis tests.
Whitney Lowe:
Yeah. there's a few other tests that we can do for the piriformis muscle that are sort of designed to be identifying piriformis syndrome. Again, entrapment of sciatic nerve involvement that might occur in this region. So they primarily target the piriformis muscle. Again, this can get into a whole nother can of worms of something that we may well delve into in another discussion some other day. But a lot of people only talk about the sciatic nerve-
Til Luchau:
That's never scared us before. Come on.
Whitney Lowe:
A lot of people talk about the sciatic nerve being compressed or irritated by the piriformis muscle. And that is certainly a potential problem, but there's also a number of other muscles in this region that can also be impacted and affected that might show up with some involvement when you do that. There's the superior gluteal nerve. There is the inferior gluteal nerve, the postural femoral cutaneous that we mentioned earlier, pudendal nerve. Lots of them in there might show up being somewhat symptomatic when you do some of these tests that really kind of zero in on the piriformis muscle, especially the sideline piriformis test, which is also called the FAIR test, sometimes. F-A-I-R is an acronym for flection, adduction and internal rotation. And then the seated piriformis test, which sort of contracts the piriformis muscle, as opposed to stretching it.
Til Luchau:
Now, I do one where you pull the knee to the chest and pull it across the midline. Is that one of those?
Whitney Lowe:
That's going to be the pretty much the same position as the FAIR test, the flexion, adduction, internal rotation. There's some fascinating things about piriformis anatomy and kinesiology that, again, we're maybe going down a completely different rabbit hole, but I got stumped by this one day, this was many years ago and looking at this. Because I was like, if you look at that piriformis stretching position, like you mentioned there, that particular position or the one that's used in the FAIR test, the traditional FAIR or sideline piriformis test, you notice that the piriformis is internally rotated, excuse me, and oftentimes laterally rotated in that stretching position. You sort of bring that leg-
Til Luchau:
The piriformis itself is rotated, or the femur?
Whitney Lowe:
I mean the hip. The hip. The femur is laterally rotated.
Til Luchau:
Okay. Got you.
Whitney Lowe:
You bring the femur up in that sort of position, across the body and sort of laterally rotate the femur. And I got stumped by that one. I was thinking, wait a minute, the piriformis is a lateral rotator of the hip, why are we stretching the piriformis if we put the hip into lateral rotation? That doesn't make any sense. And then a number of years later I stumbled across this, I think in Donald Newman's kinesiology book, a description of the piriformis' action and noted that it changes action after about 60 degrees of hip flexion because of its attachment point and becomes an internal rotator and then, therefore, stretches in external rotation as you bring that hip up into the position that you're talking about.
Til Luchau:
Yeah. I can just feel it sitting here talking to you. If I bring my hip up and just do that kind of pigeon type pose, external rotation, that's clearly stretching my piriformis, but yeah, I never put those two together that that's... What is that doing, stretching that "lateral" rotator? Even in lateral rotation.
Whitney Lowe:
Right, in lateral rotation. Yeah. So, one of those, well, a couple of these piriformis test, like the sideline piriformis test, focuses on stretching the piriformis muscle to see if it is pulling it taut and compressing those nerves. There's another test where you're basically seated and doing a resisted bilateral hip abduction, where you're trying to abduct your hips against resistance from a seated position and that's-
Til Luchau:
Does that include a belt or something or a band around the knee?
Whitney Lowe:
No, the way we do is the client is sitting on the edge of the treatment table and you place your hands on each side of outside of their knees and tell them to push their knees away from each other, and you offer resistance to that.
Til Luchau:
Interesting.
Whitney Lowe:
That's called the Pace abduction test and it's basically contracting the piriformis muscle. But sometimes I like or prefer to use some alternative positions for some of these, because you're sitting on your piriformis at that time, as well. And so if you really want to determine, make sure-
Til Luchau:
... to remove your wallet from your pocket.
Whitney Lowe:
Yeah. Remove your wallet, give it to your therapist to hold and they'll decrease the size of the wallet so it's not-
Til Luchau:
It's that wallet syndrome. We know how to reduce that. That's right.
Whitney Lowe:
... so it's not compressing your piriformis muscle. But that could be done in a supine position, too, where you just have them bring the hips into a flex position and then try to abduct them away from each other. So yeah, those are a couple of variations, but just do remember, and we talked about this in one of our previous episodes about the accuracy of some of these special orthopedic tests, that this is not rocket science. And in particular I do not advocate people use these tests in isolation without a very detailed history, much more thorough physical examination, very detailed palpatory examination and all these other things that will contribute valuable information in there.
Til Luchau:
Well, you're giving that disclaimer because they give the illusion of like, "Oh, I got it. I know what it is now." And, in isolation, we don't. It might be, at best, a working hypothesis or a place to start. And they're really fun. I love those tests. But their reliability, in terms of being able to check out and confirm the diagnosis in other ways, is varied. It's super varied. It's mixed. And it's just great to remember that, that they're fun for hypotheses, but don't take them literally.
Whitney Lowe:
No. And in my experience and this is something I'm going to try to probe probably a little bit more with Stuart McGill when we talk to him, is that I think, in many instances, those tests are used as a substitute for a detailed and thorough physical examination. I don't like that. I think that's short circuiting it and it's really decreasing the accuracy of what we can potentially do with people.
Til Luchau:
It's true. It's so hard to teach the big picture or especially to get people interested in the big picture. I mean, if I put an ad out there for a quick test that shows you where to work, that's going to get some results. If I put an ad out there that says "Detailed clinical examination, long conversation with your clients, sign right up," it's going to be a little less.
Whitney Lowe:
"Learn how to think critically."
Til Luchau:
There you go. Not a big seller.
Whitney Lowe:
Zero enrollments for that one, too.
Til Luchau:
That's it. That's it. You and me, I'll come.
Whitney Lowe:
Yeah. Okay. Right.
Til Luchau:
Anyway, so piriformis, you mentioned some tests that probably stretch the piriformis or tension it in ways that, if they light up the pain, can give us a clue that that might be involved. Do you know this one, that some people say 30% of people have an alternative pathway for their sciatic nerve?
Whitney Lowe:
Yeah. It's something that we didn't address at all. And that one, when I learned that, it just was quite fascinating and both just stumped me when you look at those anatomical variations. I think there's a good bunch of people that have their sciatic nerve going right through the middle of that muscle. Why isn't that thing just screaming in pain all the time? It's pretty amazing.
Til Luchau:
Yeah. When I learned this, this is like 1980 something, early '80s, we learned sciatica was either because of the nerve roots or because of the piriformis. And in some people the piriformis went around the nerve, which it does in a certain number of people, and that that caused sciatic pain. Well, you might know this, too, but the imaging studies of that situation don't show a higher incidence of sciatic pain in that population.
Whitney Lowe:
Yeah, that's right.
Til Luchau:
So it's not a structural problem. Some people have sciatic pain there, whether it goes through or around or in between the nerve, but it's not necessarily a statistical correlation that we always to worry about.
Whitney Lowe:
Yeah. And it reminds us, too, that despite the fact of what we see in many anatomy books, there's lots of places throughout the body where nerves go right through the middle of a muscle and don't have pain. And to me that continues to be sort of mind boggling. With all the things that we see that produce neural pain from even relatively low levels of compression over a long period of time, the fact that you have so many of these nerves going right through the middle of a muscle that don't produce pain is interesting.
Til Luchau:
Well, it just says to me that structure and shape is just one factor in pain and sensitivity. And maybe not always the main factor, even.
Whitney Lowe:
Yep. Yeah, indeed. So what else have you got on treatment things here?
Til Luchau:
Well yeah, I was going to say there are some other places, too, in the hip, in the posterior gluteal region, where it seems to be helpful to work and maybe it's because they do cause entrapment, like between the quadratus femoris. That's another place, it's like a little platform there that the sciatic nerve can sit in. And it seems to be something that can irritate or squeeze, perhaps, the nerve there, so that's something I think about. It's a little lowered down on the femoral shaft than the piriformis attachments, per se.
Til Luchau:
And especially, this is one that I just found in my practice, because I used to get quite a bit of sciatica, so working on myself there, getting people to work on me and then starting to do it with my clients, just working the intermuscular septum in the back of the legs, between the hamstrings and the adductors, gave me a lot of relief and conventional thinking would say you're just working on the place that hurts and maybe the entrapment irritation is up in the spine.
Til Luchau:
That's probably true sometimes, but there's an Italian paper and I'll see if I can dig up the reference that actually found a bunch of entrapments in the back of the leg in people whose pain got better when they addressed those locally. And that's definitely been my experience, to sometimes just work in the back of the leg where it hurts, even if it is static or pseudo sciatic or whatever, it seems to make quite a bit of difference.
Whitney Lowe:
Yeah. There was a paper I came across a number of years ago that found a pretty high correlation between hamstring strains, or prior hamstring strains, and adverse neural tension in the sciatic nerve, where-
Til Luchau:
There you go.
Whitney Lowe:
... the healing hamstring strain had scar tissue tethering the nerve and impacting its mobility and therefore leading to increases in sciatic nerve involvement. And also, just as a note, this is one of the potential causes for recurrent hamstring strains is the fact that you have irritation of that sciatic nerve, possibly after a strain, and scar tissue may be binding that nerve, preventing its mobility. And then that whole area becomes sensitized and the hamstrings become even more hypertonic and potentially prone to stress damage or muscle strain over long periods of time, because they're already hypertonic and over-contracted.
Til Luchau:
Interesting. Or density of that tenderness area or the intermuscular septum where the sciatic nerve runs. It runs in a big chunk of fascia right down the middle of the back of your leg. And again, if you have a hamstring strain or something, that scarring could just change the sliding ability that nerve through that dense connective tissue.
Whitney Lowe:
Yep.
Til Luchau:
Okay. So do you think, just in terms of things to mention, do you think that the nerve root-related sciatica is more common or sciatica related to somewhere else down the nerve, what I'm calling appendicular nerve? What's your guess or hunch about that?
Whitney Lowe:
Probably, if I had to guess, I would guess that it's probably more common with other factors other than nerve root involvement. And again, I don't have good data to back that up, but just the very fact that we've got so many other things that may produce that in creating the sort of what you call appendicular sciatic involvement, compared to just nerve root alone. That would make me play in that direction, I think.
Til Luchau:
Think that's the direction I guess, too. And I'm still guessing. And I've actually dug into that question, which is more common, appendicular or axial sciatica? And I found studies that point to both. I have. A lot of disciplines just assume that static pain means nerve root and equate that even with disc involvement. There's some studies showing that that is a really predominant cause of people's sciatic pain. But there's others that say maybe it's two-to-one the other way, two times as much peripheral sciatic nerve sensitization as nerve sensitization.
Til Luchau:
I think in my practice, though, of just the people that I have had walk in over the years, my guess is it's a lot more peripheral than axial. Maybe if I was in like a spinal clinic or something, it might be different, for example.
Whitney Lowe:
Well, I think this also comes back to how is that being evaluated? Because I think a lot of the methods of naming this and evaluating this are incomplete, because they're not doing, in many instances, as thorough of an evaluation investigation. For example, we've known for a long time that disc herniations exist in many people asymptomatically. So let's say part of your study group there has sciatic-type pain and they get an imaging study and they find a disc herniation at L4/L5 or something like that, and make then the jump, "Okay, then this person has nerve root involvement because they have a herniated disc at that level." But we do know that people can have those disc herniations that don't produce pain so that's not necessarily the indicator all the time.
Til Luchau:
At age 50, 80% of us have measurable disc degeneration. Oh, sorry. Not 80% of us. 80% of asymptomatic 50-year-olds. Just the people that don't have pain, 80% of those have disc degeneration.
Whitney Lowe:
Yeah. Pretty remarkable. And I think that skews a lot of the statistics of frequency of these kinds of things, because I do think a lot of them have been put in the bucket of nerve root-generated pain. And that's also, as we noted, too, and Gordon Waddell speaks about this a lot in his book, The Back Pain Revolution, about the dynasty of the disc, and how that led to so many decades of extensive back surgery, which was probably unnecessary for most of those people.
Til Luchau:
Yeah. Did he come up with that term, do you think? I've heard that talked about.
Whitney Lowe:
The dynasty of the disc?
Til Luchau:
Yeah. I think I even wrote about that a little bit in my book. Yeah. But that's a good one.
Whitney Lowe:
I don't know if he kind of coined that term, but I know that's where I encountered it, from him.
Til Luchau:
And that age seems to have passed, but still, maybe they estimate 4% of back pain is disc related. It's still a guess at this point. Here's another one. Piriformis syndrome, six times more frequent in women than in men.
Whitney Lowe:
Ah, no, I didn't know that one.
Til Luchau:
Yeah. Piriformis syndrome. But lumbar disc issues are twice as common in men than women.
Whitney Lowe:
Yeah.
Til Luchau:
So there's some gender differences there, too, where we might-
Whitney Lowe:
Do you have a rationale for that? That's interesting.
Til Luchau:
Well, rationale. Yeah. It is also occupation related, like truck drivers have 10 times the incidence of disc-related pain than general population. So it might be occupations or activities. Who knows?
Whitney Lowe:
Yeah. Yeah. Certainly those long, long term compressive loads in certain types of seats and things like that, we probably find that a fair amount in a certain number of the sedentary office workers as well, sitting in poor chairs and things like that, because we know a lot of those positions do increase compressive loads on the lumbar spine, inappropriately in many instances.
Til Luchau:
Yep. That's great. It's most common in people 40 to 60 years of age, meaning after 60, it gets less common.
Whitney Lowe:
Oh, you and I are over the hump.
Til Luchau:
That's right. We're on the improving side, improving curve.
Whitney Lowe:
Oh, good. One thing's getting better.
Til Luchau:
Yeah. Experienced by 40% of all people sometime in their life, with up to 5% of the population having sciatic symptoms at any given time. Here's an important point. Neuropathic rather than nociceptive, meaning it's an irritated nerve as opposed to other tissue generating a nociceptive signal. That's it, in terms of the facts. In terms of treatments or things that we talked about, all the different variations of the sliders, those are so useful to hydrate the nerves.
Til Luchau:
The evidence is mixed. There's some good studies that show a big improvement and people that do sliders. And I'll put one of those in particular, an exercise that was very carefully compared to some other sliders and seemed to have a higher level of effectiveness. But overall, sliders help some people a lot. Other people, they don't seem to help much.
Whitney Lowe:
Can you give us just a brief kind of definition of sliders, for people who aren't aware of it?
Til Luchau:
Well, that straight-leg test is a slider. You raise the straight leg and it slides the nerve through the nerve root and that is thought to maybe hydrate the nerve. Maybe it frees it mechanically so there's more mobility there. Maybe it changes the sensation so it normalizes sensitivity in a way. It could have other effects, descending modulation, things like that. But something that slides the nerve in the surrounding tissues.
Whitney Lowe:
Yeah. Okay.
Til Luchau:
And then there's variations with the head, with the bent knee, with the ankle, with the angles of the hip, all kinds of things there, with the juggling, the bike riding I mentioned, et cetera, that basically can get that nerve sliding. Or tensioning is the other thing, the Shacklock dichotomy between the two. Are you tensioning it or are you sliding it? Are you pulling it from both ends or are you pulling one end at a time? With the both ends, like dropping your head and straighten your knee, being a tensioner, which can be more aggravating, that's where you were saying, "Let's not push this thing that's hurting."
Whitney Lowe:
Yeah.
Til Luchau:
But alternating, drop your head as you bend your knee, straighten your knee as you raise your head. That basically slides that whole nerve track caudally and cranially in a way that can be relieving or calming.
Whitney Lowe:
Yeah.
Til Luchau:
So yeah, I'll put those in there. A couple of pictures of that.
Whitney Lowe:
And I would just put a plug in here, too, for why it is helpful to understand some of these facets of neural mechanics, because that may help you choose which one of these approaches you think is going to be most beneficial to somebody. Are they going to, at this stage of their game, benefit more from a tensioner versus a slider? Or what's going to be most helpful for them where they are at this particular point? Because there really isn't a blanket recipe and routine that you say, "Okay, people with neural problems, get this."
Til Luchau:
That's right. Well, especially since it's a problem that people experience chronically, it seems to go on for many people over time, it's also super important to get people to track the results of what they try.
Whitney Lowe:
Yeah.
Til Luchau:
I think of the guys, you talked about your leader client, this was a guy who rode his Harley to his sessions and it was a couple sessions before I got him comfortable enough even to take off his rodeo belt. I mean, maybe we need to explain a rodeo belt, if you're not in the West here. A rodeo belt's like a big fat leather belt with a gigantic belt buckle in front.
Whitney Lowe:
About the size of a manhole cover.
Til Luchau:
That's it. So, forget taking off his blue jeans. He wasn't going to do that. But I got him to take off his boots, take off his rodeo belt at some point. And he had such painful sciatica that it was quite a challenge to work with. I got it calmed down in a great way and sent him home. It did seem to be pretty piriformis related. I sent him home with a tennis ball and showed him a couple of moves, just to lie on the tennis ball and move his leg around and it seemed to really help.
Til Luchau:
So he came back a couple times later. It flared up because he'd fallen asleep on the tennis ball. Obviously, it felt so good that he just kind of overdid it. I learned such an important lesson there that it's all about dosing and it's all about doing a little bit and seeing how it responds.
Whitney Lowe:
Yep. Yeah.
Til Luchau:
And once it's flared up, it's harder. It's harder. You got to give it time, keep moving a little bit, but you don't want to keep poking the dragon, or whatever it is.
Whitney Lowe:
Exactly. Yeah, yeah, yeah. Yeah. Poking the bear.
Til Luchau:
Poking the bear.
Whitney Lowe:
Yep. All right. Anything else that we need to [inaudible 01:05:26]
Til Luchau:
Oh, I got so much. I got so much. But I think that we covered the bases there. We covered the main points. The rest is just more technical stuff that's easier to see than to talk about so I'll put a couple of pictures in the handout and then yeah maybe people will come to the training, too, or check out one of the other things. You mentioned some understanding neuro dynamics. Do you have anything in your repertory classes that-
Whitney Lowe:
Yeah, we definitely explore those things in both our cervical, lumbar and pelvis classes, all three of those courses, because of the role of these tissues. We explore some of the neurodynamic testing both from the evaluation and treatment standpoint, as well, so yeah.
Til Luchau:
Great. We'll put some links in there to your site, et cetera, but maybe this is a good time for our rollout for our closing sponsor.
Whitney Lowe:
Yes, indeed. And who is that today?
Til Luchau:
Well, in addition to me, since I'm kind of sponsoring this episode with our sciatica-
Whitney Lowe:
That's right.
Til Luchau:
Let me do that plug first. The Sciatica Live Stream course August 12, 2022, or later by recording, if you're listening to this later, and if you're a listener to this podcast, which if you've made it this far, you qualify, you can save 15% by entering "Thinking" at checkout, at advanced-trainings.com. Now, our other sponsor, our rollout sponsor, is Handspring. And when I was looking for a publisher for a book I wanted to write, I was fortunate enough to end up with two offers. One from a large international media conglomerate and the other from Handspring, which at the time was a small publisher in Scotland, run by just four people who love great books and who loved our field.
Til Luchau:
To this day, I'm glad I chose to go with Handspring, as not only did they help me to make the books I wanted to share, the Advanced Myofascial Technique Series, but their catalog has emerged as one of the leading collections of professional-level books written especially for body workers, movement teachers, and all professionals who use movement or touch to help patients achieve wellness.
Whitney Lowe:
And Handspring recently joined with Jessica Kingsley Publishers' Integrative Health, Singing Dragon imprint, where their amazing impact continues. So head on over to their website at handspringpublishing.com to check their list of titles and be sure to use the code "TTP" at checkout for a discount. So thanks again so much, Handspring, for continually supporting the Thinking Practitioner podcast. And we do want to say a thank-you to all of our sponsors. And of course also to you, the listeners. We appreciate you hanging out with us and hope we've shed some light on some interesting things for you.
Whitney Lowe:
As a reminder, you can stop by our sites for show notes. And this one, we do have a handout available and we'll put that at the bottom of the show notes where that handout is available. So that'll be coming off Til's site, I believe, so thank you for that, Til. You can find other information on our show from our websites. Mine is academyofclinicalmassage.com and Til, people can find you where?
Til Luchau:
advanced-trainings.com. If there are questions or things you want to hear us talk about here or feedback you have for us, quibbles, complaints or spontaneous remissions, anything else you want to tell us about, email us at info@thethinkingpractitioner or look for us on social media, just under our names. My name is Til Luchau. Whitney?
Whitney Lowe:
And I will be also found on social media under my name, Whitney Lowe. And if you will take a moment, if you can, rate us on Apple Podcasts, it does help other people find the show and then helps encourage us to keep at it here for a while. You can also hear us over on other platforms, Spotify, Stitch, or Google Podcast, or wherever else you happen to listen. So please do share the word and tell a friend. Thank you again so much for listening and we will see you again here shortly.

Live Workshop Schedule
Stay Up to Date
...with the Latest Episode, News & Updates
Get our free Techniques e-Letter
You'll occasionally receive the latest schedule updates, tips, secrets, offers, resources, and more.
Check out our ironclad privacy and SMS policies. You can unsubscribe/stop at any time.
This Month's Free Online Course
Our gift to you. Includes CE, Certificate, and Extras.
Follow Us
Join us on FaceBook, Instagram, Twitter and YouTube
for information, resources, videos, and upcoming courses!






0 Comments